Primary Options for Acute Care (POAC)
MidCentral Region
*NEW*
Major Cellulitis Health Pathway
- Removal of IV antibiotics in the community — high dose oral antibiotics, particularly boosted with Probenecid, are more effective than once daily IV dosing.
- Watch the Cellulitis Webinar that Tu Ora - Compass Health recorded when they introduced similar changes in 2021.
- Familiarise yourself with the pathway before you need to use it.
- Keep an eye out for an upcoming interprofessional education session.
- Review the outcomes of this study:
Oral antimicrobial therapy for cellulitis versus outpatient parenteral antimicrobial therapy: a single-centre audit of cellulitis outcomes
Click on each of these links to take you to the relevant section on this page:
Primary Options for Acute Care (POAC) is a patient centered service which enables General Practice Teams (GPT) to safely manage acute illness, by accessing an increased range of specified services in the community. This service provides an alternative to referring patients to the Emergency Department (ED). Referrals can be made directly to POAC by a health professional, or to discuss a case please call the Acute Care Team.
Programme Objectives
- Enable primary care providers to maximise the management of patients in the community, within the constraints of the funding rules.
- Create opportunities to improve the primary-secondary interface.
- Develop and implement new care pathways to reduce acute demand.
- Link with other community services that support the overall purpose.
- Reduce number of bed days with an early discharge service.
- Support a framework that provides an integrated approach to the patient care, improving the patient experience and delivering healthcare services that are timely and convenient.
- Facilitate increased capacity and capability for primary healthcare to provide safe acute care in the community.
While the Doctor or Nurse Practitioner takes full clinical responsibility of their patients who enter the POAC service, the POAC Coordination team will be undertaking regular retrospective clinical audit and case review on specified POAC cases as triggered through the Continuous Quality Improvement (CQI) process. Through this process, feedback will be provided to sites in order to ensure consistency, eligibility criteria are adhered to and that the case was appropriate for POAC.
Eligibility
POAC is no longer condition-specific, instead there are only two criteria/questions when deciding if a patient is a POAC case:
- Would the patient otherwise be sent to ED today? The clinician can confirm that, in their opinion, the patient would have otherwise been referred acutely to hospital. This decision must be made on clinical grounds only. Patients cannot be treated under POAC purely due to a financial reason i.e. Practices providing POAC to patients who cannot afford to pay, there must be a clinical indication.
- Is it safe to manage the patient in the community? Can the clinicians take clinical responsibility for the patient?
There is now no age limit on who can receive POAC services if clinical pathways are followed, and it is safe to manage the patient in the community.
And….
- The patient has given his/her consent to the recommended treatment.
- The patient has given his/her consent to their clinical consultation notes being used for auditing and evaluation purposes as part of the data collection process for the POAC programme.
- The patient is eligible to access funded New Zealand health care services.
- The clinician can take responsibility for the patients care, or have handed over the patient to another clinician.
Other applicable funding streams (e.g. ACC, maternity, private insurance) cannot be used in the first instant.
Programme Services
A range of services are accessible through POAC, these include:
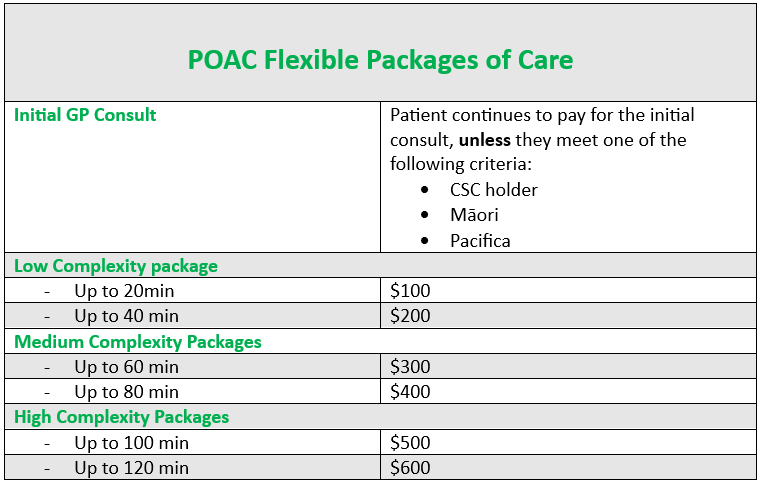
Flexible Packages of Care
POAC is claimed as flexible packages of care.
- Are no longer condition specific.
- Are no longer age specific.
- Are based on active time spent keeping the patient out of ED and thus reflect the complexity of the presentation.
- Recognises the clinical time spent whether this is consultation (in-person and virtual follow-up if appropriate), procedural, consumables, transport, or active observation within the primary care setting.
- Bulk-billing approach with one overall claim at the end of an episode of care instead of claiming each separate interaction with the patient
- High trust model – we have confidence that GP teams will use this system fairly, equitably, and consistently to provide community-based care to patients.
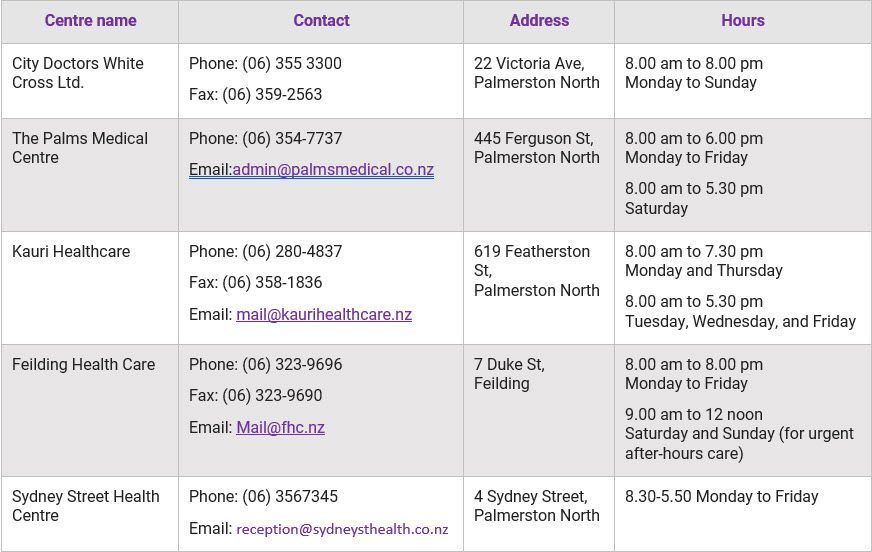
POAC Referral Centres

Please note: The referral hours at the latter end of the day indicate the latest time a patient can present to the PIAC entre in order for assessment and treatment to occur before closing.
POAC Clinical Pathways and Policies
(please note: this is not an exclusive list of conditions that can be managed under POAC but a list of common presentations)
Adult Health Pathways
Paediatric Health Pathways
Funding Policies
POAC Resources
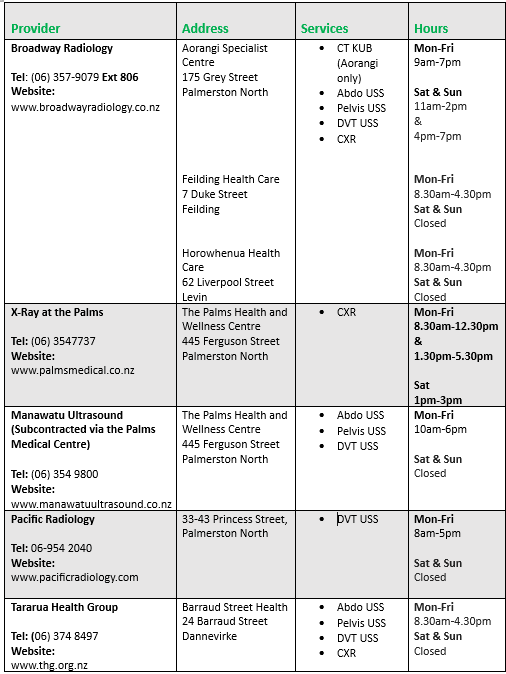
POAC Radiology
As part of the POAC expansion, we currently have wider access to same day radiology tests.
If you require assistance in coordinating a same day appointment, please reach out to our POAC Coordinator.
For POAC initiated radiology investigations, please ensure to annotate “POAC” on the request form to indicate urgency of turnaround. The only exception here is for all DVT ultrasounds should be annotated CRR not POAC.
Using the practice management system (or paper referral) generate the POAC case number and write a radiology request form. Advise the patient/carer to attend a private radiology provider of their choice with the request form.
POAC Radiology Providers
St John Redirect Pathway
POAC will support St John to redirect patients to primary care as an alternative to ED by providing funding for a consult at the nominated POAC Centre. Provided patients meet the specific criteria, their visit is free to POAC centres.
The aim is to ensure that ‘the right patients are treated in the right place, by the right person, at the right time’.
The GP/Nurse have the right to decline St John redirect to their clinic if they feel it is unsafe or they do not have the ability to see or manage the patient. If a patient is declined, St John personnel document the reason for this by using “referral@declined” in the disposition notes on the ePRF.
Please note:
St John redirect excludes Ōtaki Medical and Village Medical Centre
ED Redirect Pathway
ED staff can redirect patients to urgent care services who are deemed as being suitable for community management. Provided patients meet the specific criteria, their visit is free to POAC centres. ED redirect sites include:
City Doctors
- 8am-7pm Monday to Sunday can accept patients from all practices or unenrolled
The Palms Medical Centre
- 9am-5pm Monday to Friday can accept patients from all practices or unenrolled
-9am-4pm Saturday can accept only Palms patients, unenrolled or Palms affiliated practices (Victoria Medical Centre, Whakapai Hauora, Massey Medical)
*NEW*
Major Iron Infusion HealthPathway Updates:
- New PHARMAC SA criteria. Please ensure all practitioners completing this form are using the one attached below. POAC will ONLY fund the infusion is the PHARMAC criteria are met
- The age range has changed from 16 years down to 14 as endorsed by Paediatrics
- New 'request for Iron Infusion form' when referring to another practice for infusion
- New checklist
- New patient information link
Ferinject
POAC funding is available for patients that:
- Meet the PHARMAC criteria for subsidy by special authority
- Aged 14 years or older.
- Assessed as clinically safe and appropriate to be managed in the community.
- Eligible to access funded NZ health care services.
Please note: "Request for funded administration of IV Ferric Carboymaltose (FERINJECT) to treat Iron Deficiency Anaemia" form only needs to be completed if you are referring them to another POAC referral centre to have their infusion.
For more information including procedure please refer to Whanganui & Palmerston North Community Health Pathways-see link below.
POAC Referral Centres
ED-COPD Transition of Care Pathway
This programme is designed to improve the transition of care between ED and Primary Care for COPD Patients.
The key aims of the programme are to:
- Improve patient understanding of their condition
- Strengthen the focus on action planning
- Improve condition management and quality of life measures
- Reduce presentation to GP, ED and the risk of condition review
Funding
There is funding available to support this pathway via the POAC programme. Both the review and the comprehensive respiratory assessment are fully funded for the patient. Spirometry is also funded as part of the condition review.
Key Contacts
Dr Paul Cooper
Clinical Director of Acute Care Paul.cooper@thinkhauora.nz
(06) 3549107


